Table of Contents Show
It may look like just dry, flaky skin at first — but psoriasis runs far deeper than that. This chronic condition, marked by inflamed, scaly patches, is not simply a skin problem but an immune system disorder that accelerates skin cell turnover. According to dermatologists specialising in psoriasis treatment Singapore, early diagnosis and proper management can prevent flare-ups from worsening and help patients regain control of their skin and confidence.
Understanding Psoriasis
Psoriasis is a chronic autoimmune skin condition where the immune system mistakenly speeds up the skin renewal process. Normally, skin cells take about 28 to 30 days to mature and shed, but in people with psoriasis, this cycle happens in just 3 to 5 days. The rapid buildup of skin cells leads to thick, red, scaly patches, most commonly appearing on the scalp, elbows, knees, and lower back.
While it isn’t contagious, psoriasis can significantly impact emotional wellbeing and quality of life. Many patients feel self-conscious or anxious due to visible plaques, often avoiding clothing or social situations that might expose affected skin.
Common Types of Psoriasis
Psoriasis presents in several different forms, each with its own symptoms and triggers:
- Plaque Psoriasis (Psoriasis Vulgaris) – The most common type, causing raised, red lesions with silvery-white scales.
- Guttate Psoriasis – Often triggered by infections like strep throat, appearing as small, red teardrop-shaped spots on the skin.
- Inverse Psoriasis – Found in skin folds like underarms or groin areas, appearing smooth and shiny rather than scaly.
- Pustular Psoriasis – Characterised by white pustules or blisters filled with non-infectious pus.
- Erythrodermic Psoriasis – The most severe form, causing widespread redness, itching, and pain across large areas of the body.
Understanding the type of psoriasis you have helps determine the most effective treatment plan.
What Causes Psoriasis?
The exact cause of psoriasis remains complex, but most experts agree it’s a multifactorial condition — influenced by both genetic and environmental factors.
1. Overactive Immune System
The immune system mistakenly attacks healthy skin cells, triggering inflammation and rapid skin cell production. This immune response is what causes the redness, swelling, and scaling seen on the surface.
2. Genetic Predisposition
Psoriasis tends to run in families. Having one or both parents with psoriasis significantly increases your risk, though not everyone with a genetic link develops the condition.
3. Environmental and Lifestyle Triggers
Certain factors can trigger or worsen flare-ups:
- Stress and lack of sleep
- Cold, dry weather
- Skin injuries (scratches, burns, sunburn)
- Infections
- Certain medications (like beta-blockers or lithium)
- Alcohol and smoking
Is Psoriasis Contagious?
A common misconception is that psoriasis spreads through touch or personal contact. In reality, psoriasis is not contagious. You can’t catch it from or pass it to anyone through physical contact, shared objects, or proximity.
However, psoriasis can spread on your own body — meaning that new lesions can appear on previously unaffected areas. This is due to a phenomenon called the Koebner response, where skin trauma or irritation triggers new psoriasis patches in that area.
For example, scratching, friction from tight clothing, or even bug bites can lead to new lesions forming along the damaged skin. This is why dermatologists emphasize gentle skincare and avoiding unnecessary irritation.
How Psoriasis Affects the Body Beyond Skin
Psoriasis doesn’t just affect the skin — it’s increasingly recognised as a systemic inflammatory condition. Research shows links between psoriasis and several other health problems, including:
- Psoriatic arthritis, causing joint pain, stiffness, and swelling
- Cardiovascular disease, due to chronic inflammation
- Metabolic syndrome (including obesity, diabetes, and high blood pressure)
- Depression and anxiety, often triggered by visible symptoms and social stigma
Managing psoriasis effectively helps reduce the risk of these complications and improves overall health outcomes.
The Role of Stress and Immunity
Stress is one of the most well-documented psoriasis triggers. When the body experiences psychological or emotional stress, cortisol and other stress hormones rise, intensifying inflammation and worsening existing plaques.
This creates a vicious cycle: flare-ups cause anxiety and self-consciousness, which in turn leads to more stress — and more flare-ups. Learning to manage stress through mindfulness, relaxation techniques, or therapy can make a meaningful difference in reducing symptom severity.
How to Prevent Flare-Ups
While psoriasis can’t be cured, flare-ups can be managed or prevented with consistent skincare and lifestyle habits. Dermatologists recommend the following strategies:
1. Moisturise Daily
Keeping skin hydrated helps reduce dryness, scaling, and itchiness. Choose thick, fragrance-free moisturisers or ointments, especially after bathing.
2. Avoid Harsh Soaps and Hot Showers
Use gentle, pH-balanced cleansers. Hot water can strip natural oils, leading to irritation.
3. Protect Skin from Injury
Even minor cuts, burns, or insect bites can trigger new lesions due to the Koebner phenomenon. Use sunscreen and avoid unnecessary scratching or picking.
4. Manage Stress
Incorporate relaxation techniques such as meditation, yoga, or breathing exercises into your daily routine.
5. Maintain a Healthy Diet
Some people find that anti-inflammatory diets rich in fruits, vegetables, and omega-3 fatty acids help reduce flare-ups. Limiting alcohol and processed foods may also support skin health.
6. Follow Medical Advice Consistently
Regular follow-ups with your dermatologist ensure treatment plans stay effective and adjusted to your skin’s response.
Medical Treatments Available
The right treatment depends on the severity and type of psoriasis. Dermatologists may recommend one or a combination of the following:
1. Topical Treatments
Creams and ointments containing corticosteroids, vitamin D analogues, or coal tar help reduce inflammation and slow skin cell growth.
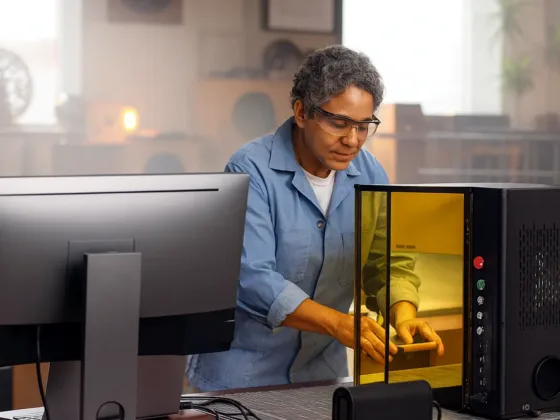
2. Phototherapy (Light Therapy)
Controlled exposure to ultraviolet (UVB) light can slow skin cell turnover and reduce scaling. Treatments are usually done in a clinical setting under supervision.
3. Systemic Medications
For moderate to severe psoriasis, oral or injectable medications target immune system activity. Examples include methotrexate, cyclosporine, or biologics that block specific inflammatory pathways.
4. Biologic Therapy
These advanced treatments use targeted proteins to suppress specific immune responses. Biologics have revolutionised psoriasis care, often leading to significant, long-term skin improvement.
5. Combination Therapy
Sometimes, combining topical, light, and systemic treatments produces the best results, especially when flare-ups are difficult to control.
Living Confidently with Psoriasis
Beyond medical management, emotional support plays a vital role. Psoriasis can affect confidence, social relationships, and even career choices. Joining support groups or therapy sessions can help patients feel less isolated and more empowered to manage their condition.
Simple steps — like wearing breathable fabrics, using gentle skincare, and maintaining open communication with your dermatologist — can make daily life more comfortable and reduce flare-up triggers.
When to See a Dermatologist
You should seek professional evaluation if you notice:
- New or worsening patches of red, scaly skin
- Painful or bleeding plaques
- Nail changes such as pitting or discoloration
- Joint stiffness or swelling
- Persistent itching or irritation not responding to over-the-counter treatments
Dermatologists can confirm the diagnosis, identify potential triggers, and customise treatment for your unique skin type and lifestyle.
The Takeaway
Psoriasis isn’t contagious — but it is complex, chronic, and deeply linked to the body’s immune system. By understanding how it develops, what triggers flare-ups, and which treatments can help, patients can take proactive control over their condition.
If you’re struggling with recurring or severe symptoms, consider consulting a dermatologist experienced in psoriasis treatment Singapore. With proper diagnosis, personalised care, and long-term management, clear and comfortable skin is within reach.